 This episode follows on from ‘Managing persistent short-term absences’ and will focus on managing staff on long-term sickness leave.
This episode follows on from ‘Managing persistent short-term absences’ and will focus on managing staff on long-term sickness leave.
First of all, what constitutes a “long-term” absence?
Four weeks. It’s that simple. Any absence lasting four or more calendar weeks is deemed to be “long-term”.
Why is managing long-term absence any different?
Essentially, it doesn’t have to be. As per managing persistent short-term absence, you still have a policy to follow. But the nature of most long-term absences means there’s more to consider.
Long-term sickness can be more complex as we’re talking about illnesses that are more serious. The main three reasons for long-term illness in most organisations are musculoskeletal problems, stress/anxiety/depression and planned surgery. The principles that relate to managing the absence shouldn’t change because of the illness type, but the journey you take may differ.
For example, if an employee is absent due to surgery, you’ll have an idea of how long they’ll be off for, what the problem is and what sort of adjustments you’ll need to make on their return. You’re also more likely to be confident that the employee is going to return to work after a period of recovery.
With other types of illness, you may not know how long the employee will be off work. They may be trying a number of treatments/therapies to see what helps. They might start to improve, start planning a return to work and then face a setback which changes everything. They may be diagnosed with something from which there’s no recovery. You must be prepared for many possibilities.
Why do we have to manage long-term absence?
Sounds like a stupid question, but you’ll be surprised how often I’ve heard this when working in HR, mostly from the employees. “Why can’t you just leave me alone? I’m off sick!”
Firstly, let’s consider the impact of the absence. As managers, we need to know how long employees are likely to be absent as we need to arrange cover, reallocate work, etc. We need to inform the team, let Payroll know and make sure someone’s covering the role.
Secondly, because even if the employee thinks they’re not coming back, I can’t replace them while they still have a contract. If they’re technically still employed, I can’t give their job to someone else. So a process needs to be followed.
What are the key things to do in managing long-term absence?
Contact
You must maintain regular contact with an employee who’s off sick. Some managers are nervous about contacting staff for fear of being accused of harassment. But if your sickness policy states that staff must maintain contact with management during any period of absence, you’re covered!
I tell my staff that they must contact me every day for the first three working days of absence. This must be by phone, and I need to know the reason for the absence and when they think they’ll be back. If they know from day 1 that they’ll be off for a week or more, then we’ll agree a contact plan.
In that phone call I want to know how they’re doing and what sort of treatment or support they’re getting and how effective it is. I’ll update them on what’s happening at work. We can discuss when they think they might come back and what, if anything, they might need to assist them. If we haven’t set a date for returning, I’ll confirm the date of the next contact.
Occupational Health Input
Occupational Health plays a key role; their report will affect how you take things forward. So you want to be sure you’ve got all the information you need. Key questions to ask include:
- What is the reason for the employee’s absence? (NB: I’ve had occasions when the Occupational Health physician has told something different to the employee!)
- What treatment is the employee receiving for their illness?
- Are there any reasonable adjustments that could be implemented to aid their return to work?
- Would the employee’s illness be classed as a disability under the Equality Act 2010?
- Do you see the employee being able to return to work within the next few weeks?
I’d include details of the employee’s role, contracted hours, working environment and any previous history of sickness absence, as well as any supportive measures already being implemented.
What should you do if the employee refuses to consent to an Occupational Health referral? We can’t force them. However, it limits THEIR options more than ours. The response I’ve always given to the employee is that if they refuse to see Occupational Health or allow us to write to their GP, then we can only go on the information we have. And if the information is that the employee is too unwell to work and they can give no indication as to when they can return, we’ll have to proceed based on this information alone.
Helpful resources: The Staff Occupational Health Policy [PLUS] explains why staff may be referred to OH and the referral process, referencing relevant additional guidance throughout. Further absence management resources can be found here.
Reasonable adjustments
Everyone associates this phrase with disability, and they’re right. But in the context of employment, how do we determine if someone’s disabled?
NB: In an employment tribunal, a disability is determined by a judge, not a doctor! The definition we try to adhere to asks whether a condition puts a person at a physical or mental disadvantage for a period lasting longer than 12 months.
This sounds rather woolly, so err on the side of caution and if there’s something that can be identified as being at least an “underlying health condition”, which has been an issue for more than 12 months, consider reasonable adjustments. Occupational Health will tell you if they think something might be classed as a disability, but it’s up to you to decide whether you want to fork out for a referral just for that!
Reasonable adjustments shouldn’t be dependent on an employee going off sick for you to consider implementing them. As soon as you’re made aware of an underlying health condition, you should discuss with the employee what, if any, reasonable adjustments may need implementing. I’ll cover this in more detail in my next blog, but here are some examples that can be offered to aid the return to work of an employee who has been on long-term sick leave:
- A phased return: Returning to work can be exhausting if you’ve been off for months. Many staff returning from long-term sickness who don’t have a phased return end up going off again in a relatively short time frame.
- Temporary redeployment/amendments to duties: If a particular element of the role is going to be a challenge or a barrier to the person returning, take it away for a while. (Someone else has been doing it while they’ve been off anyway.) Gradually reintroduce these tasks once the employee has found their feet.
- Temporary change to working pattern/shift times: The employee may need to attend appointments as part of their treatment, or they may find it hard to get up early, or they may tire later in the day. Try to accommodate a temporary change until they’re back in the swing of things, or if possible make a permanent change but make it subject to review.
- Change of work location: If the employee needs a quiet space to work, or has problems with the light in a particular area, can you move them somewhere else?
In my next blog, I’ll explore different types of reasonable adjustments and how to make effective Occupational Health referrals.
Meetings
If the employee’s absence hits the four-week point, it’s time for a meeting. (The only exception would be staff who’ve had planned surgery. In those situations I’d be maintaining phone contact as above.)
Explain to the employee over the phone that as the absence is now long-term and there’s no confirmed return-to-work date, you need to arrange a review meeting.
This makes people nervous, so I’d explain that whilst it’s a formal meeting, the aim is to see how things are going and what we can do to facilitate a return to work. Offer them the opportunity to have a union representative or colleague with them. (I’d advise against allowing relatives/friends to attend as they don’t always remain professional!) Send them a letter inviting them to the meeting. A variety of template letters can be found here.
The meeting could be one of many. But hopefully not too many! Each meeting should discuss:
- The employee’s health issue
- Any progress they’ve made or any barriers to progress
- What support the organisation can offer
- Whether there’s going to be a return to work in the foreseeable future
Each meeting should identify the next steps to be taken and every meeting should be followed up in writing.
A “reasonable” time frame for returning to work can vary from practice to practice, from role to role, and from individual to individual. But don’t feel you have to wait until the employee has been off for, say, six months or whenever their sick pay runs out. If I know that an employee isn’t going to be able to return to work, even if they’ve only been off for six weeks, I can instigate dismissal proceedings. All I need is a medical opinion confirming that they can’t predict a return-to-work date.
Taking this stance is entirely up to you. The plan I generally adhere to looks like this:
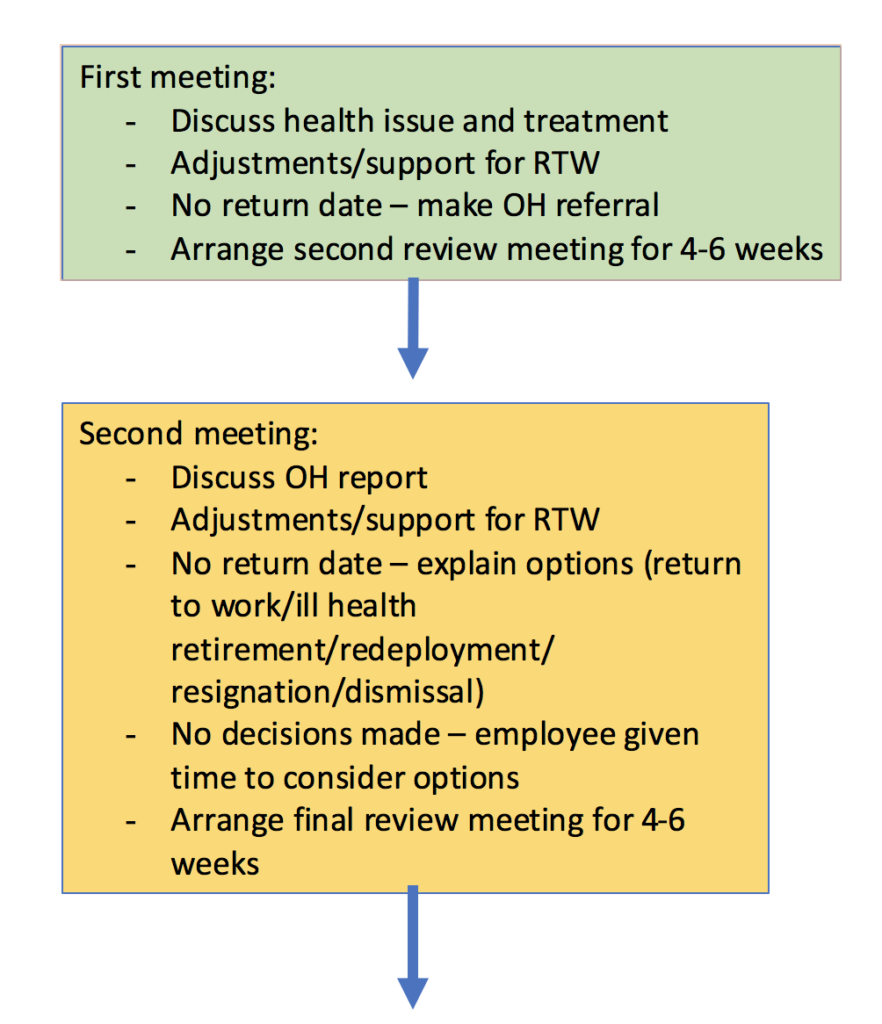
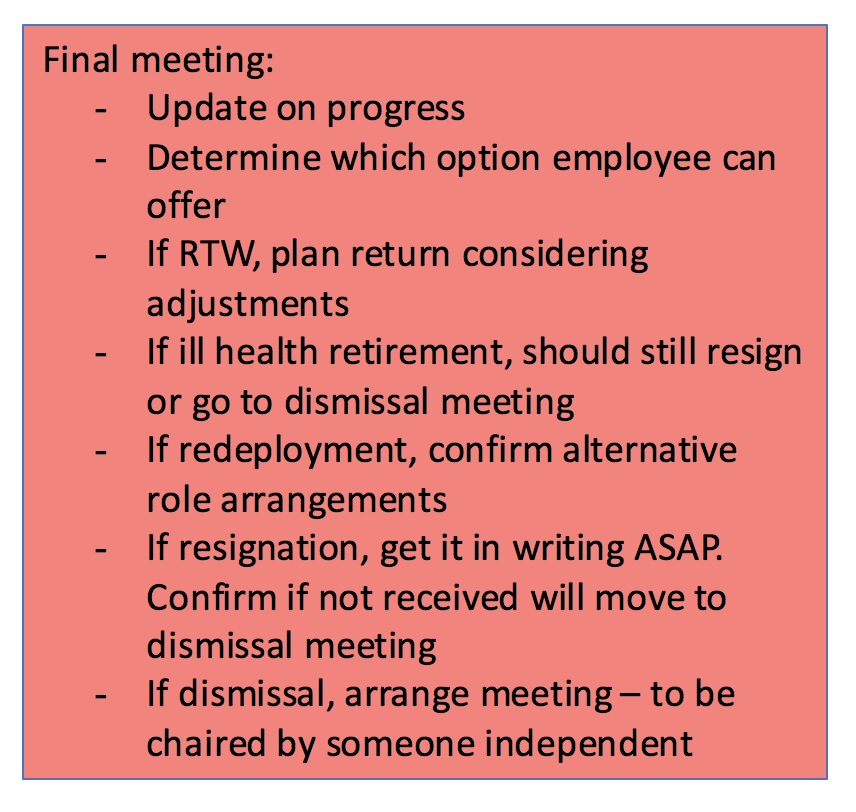
You may find the second meeting happens more than once depending on how things progress.
If you end up in a dismissal meeting, it should be chaired by someone who hasn’t been involved in the management of the absence so far (e.g. a partner) and it may need to be supported by someone else (e.g. another manager in the practice, or a PM from a neighbouring surgery). You should present to the chairperson what has been done up till now and the employee should be given the opportunity to add anything they feel is relevant. The chairperson makes the final decision.
In the majority of cases the employee will return to work in some form and dismissal will not be required. But it’s good to be prepared!
Where does it leave the employee in terms of the sickness policy?
I always recommend having a separate section in your policy for the management of long-term absence. It should explain your process for managing staff (i.e. contact, meetings, Occupational Health referrals and possible outcomes if there’s no return) and how the absence relates to your overall sickness management policy. The Practice Index Plus Sickness Absence Management Policy provides a good ready-made example!
If you have sickness targets that relate to the number of days lost or the Bradford Factor, it’s unfair to include long-term absence in those targets, as in most cases they’ll automatically trigger the breach points. This could be shown to be indirect disability discrimination.
It’s reasonable to class any long-term absence as one episode in the sickness management process (e.g. so if three episodes and/or a working week constitutes a breach, the long-term episode is one of the three episodes, but you don’t count it in the working week section). This can also then be classed as a reasonable adjustment. As I said before, err on the side of caution!
Key point to remember
Do NOT leave long-term sickness unmanaged. You, as a manager, have a duty of care to your employees and to your organisation. Make contact, be clear about expectations, offer support and if there’s no return to work, take appropriate action.
If you have any questions, please post below and I’ll respond. Thanks for reading!
For parts one and three of Top Tips for Managing Absence, click here.
———–
Topics trending in the forum:
The dreaded FLUAD again!
Working from home and just had the dreaded message!
Another PPG headache
Exit interview
Pneumo ordering





0 Comments