Data analyst Stephen Black offers some insights into how changes in workflow and GP and patient behaviour are taking place following the widespread adoption of online consultations in general practice.
Data from NHS England says that, as of 24th April, 58% of practices are now live with an online consultation system. The data also confirms that 98% of practices have a system for video consultations in place.
For the majority of practices this has been a massive leap into unknown territory, driven by the arrival of COVID-19. Now they’re all signed up, will practices be able to make the most of the features these online systems have to offer? And will the systems allow practices to genuinely transform the way they provide patient care?
Time will tell as stories begin to emerge from practices keen to share their experiences of online consultations. In the meantime, at ‘askmyGP’ we’ve made our extensive data publicly available to highlight the changes online triage have brought to the practices we’re working with. Here are some observations based on our aggregated data, which we’ve been collecting since 2018.
Peaks and troughs of patient demand
Every day the system currently manages 10,000-15,000 remote consultations, covering 156 practices with 1.5 million patients at the time of writing – these figures are increasing daily. The start of the week remains the busiest time and the system is currently managing between 2,500 and 3,000 incoming patient requests between 8:00 and 9:00 on a Monday morning.
However, the data for incoming patient requests by day and by hour shows a significant change as a result of the pandemic. The peak in demand is a little later in the day, and is more spread out across the day, making it easier for practices to manage demand.
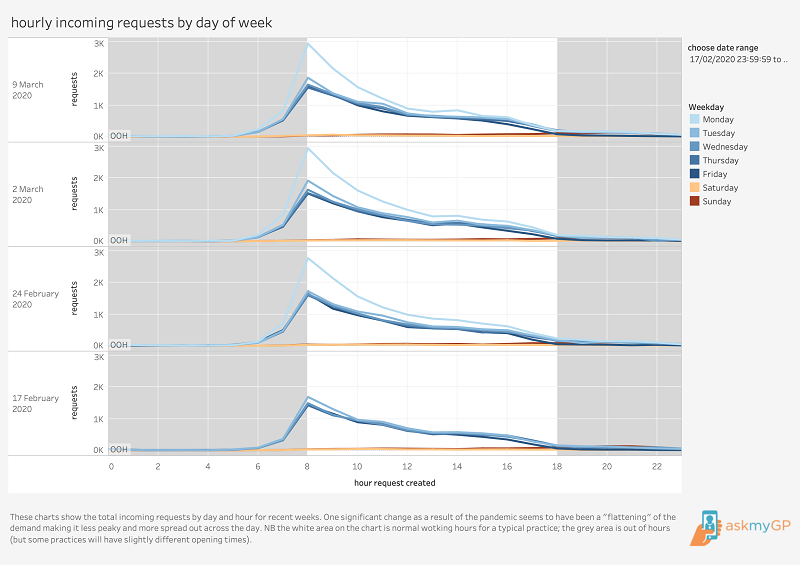
Hourly activity pre Covid-19
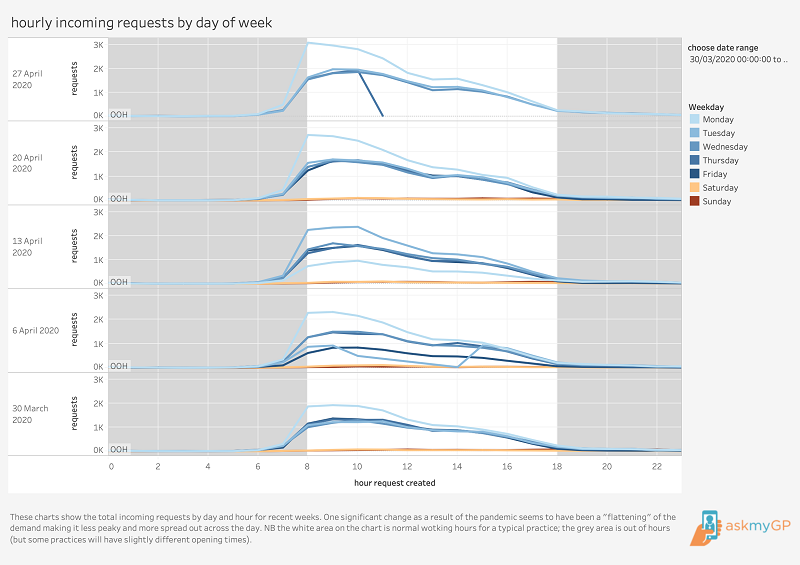
Hourly activity post Covid-19
How are patients getting in touch?
In the 10 weeks to 15th March, just under half a million incoming patient requests were processed. Typically, 32-35% of patients made requests by phoning the practice. As concerns about COVID-19 have risen, more patients have made their requests online through secure messaging, and phone requests have dropped to 22-28%.
When patients go online, they type a message telling the GP about their problem in their own words. Patients who don’t have internet access or who don’t want to go online can contact the practice by phone. In this case the practice processes the patient’s request through the system. This means that, for most practices, the system tracks 100% of incoming patient requests.
How are practices responding to patients?
When patients contact the practice, they’re given the option of choosing which way they’d like the doctor to contact them. The options are phone call, online message or video consultation.
However, practices don’t simply give patients what they ask for. They consider the content of the patient’s request and their condition before deciding on the appropriate response. Pre-pandemic, it was notable that only a third of patient requests from patients were for face-to-face appointments.
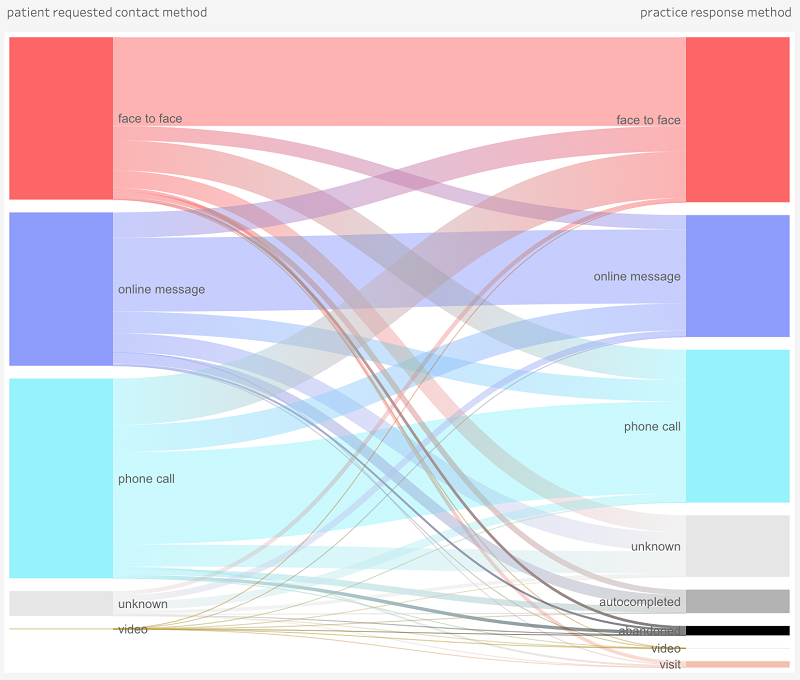
Consultation methods pre Covid-19
The chart below shows how big a change was caused in response to the virus. It covers 376,000 requests from 16th March to 27th April. What patients requested and what practices delivered have both changed radically to minimise the need for face-to-face contact.
In normal times a little over 30% of patient requests and practice responses involve face-to-face appointments. It’s now 3-4% and that change happened in days.
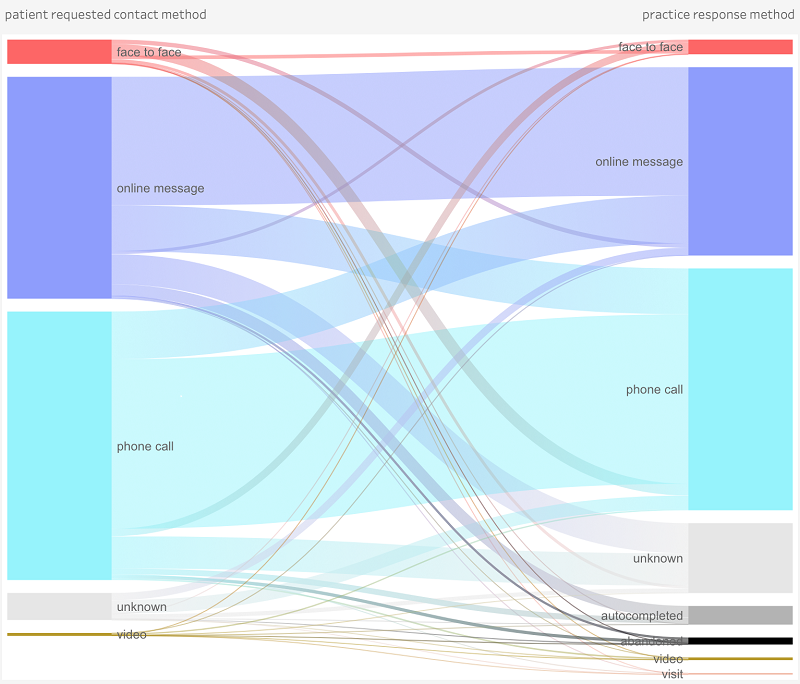
Consultation method post Covid-19
How many patients are contacting the surgery?
Another change, which is possible to see with live data, is the total number of patient requests. Typically, practices see weekly requests of 6-8% of their patient list every week. That ratio is currently running at a little over 4-5% (in aggregate it peaked at about 8% in the week lockdown was announced as patient worries about the virus caused more demand than normal).
The reduction in patient contacts is a worrying trend and practices concerned about the effect of the lockdown on other health conditions will need to encourage their patients to talk to their doctor rather than brushing aside any worries.
Four things we’ve learned
- Total triage approaches give practices the freedom to tackle work in the way they consider to be most appropriate.
- Even in normal times the systems allow GPs to give every patient an appropriate and speedy response.
- Good systems for managing total triage enable practices to respond very rapidly to major events like the current pandemic.
- Once practices see the benefits and recognise the need to change their processes, total triage can be rolled out very quickly.
Dr Stephen Black is Chief Analyst at ‘askmyGP’ and a data scientist and blogger who analyses data to improve policy-making and to improve the performance of healthcare organisations from GPs to hospitals.
Topics trending in the forum
Shielding staff
Pregnant women during COVID in workplace
Masterclass by me (@JacksonR)
Advice please





0 Comments